Lupine Publishers Group
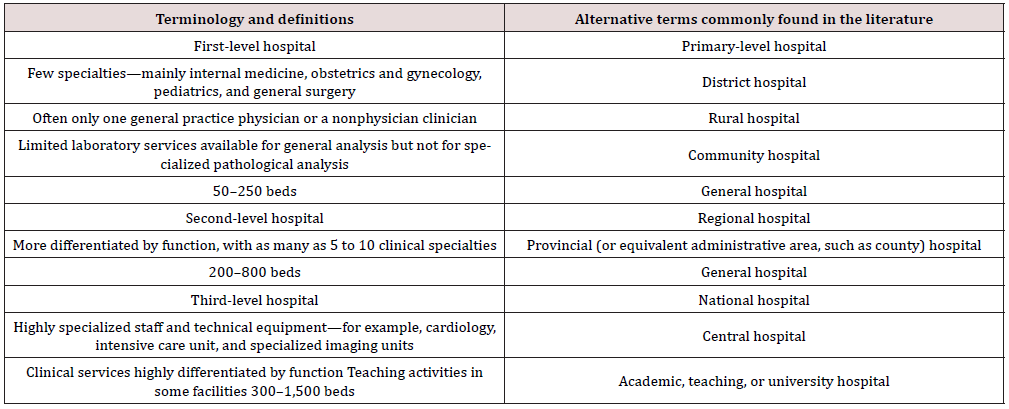
Lupine Publishers
Menu
ISSN: 2637-4722
Research Article(ISSN: 2637-4722) 
Trends of Hypospadias Surgery Amongst Pediatric Surgeons at Resource-Limited Rural & District Hospitals in Maharashtra State: An Online Survey Volume 3 - Issue 5
Jahoorahmad Z Patankar*, Hemant N. Lahoti, Ravindra Vora, Manjusha Sailukar
- Consultant Paediatric Surgeon, The Children’s Hospital, India
Received: November 24, 2022 Published: December 01, 2022
Corresponding author: Jahoorahmad Z Patankar, Consultant Paediatric Surgeon, The Children’s Hospital, Mumbai, India
DOI: 10.32474/PAPN.2022.03.000173
Abstract
Background: Hypospadias is one of the most common congenital genital anomalies for which surgery early in life is indicated. Surgeons practicing in Rural Hospitals with limited resources are faced with numerable challenges.
Aims: Evaluate current practices regarding a variety of aspects of hypospadias surgery amongst paediatric surgeons at Rural Hospitals.
Materials and Methods: Pediatric surgeons from Rural & District Hospitals in Maharashtra were invited to participate in an anonymous online questionnaire (Hypospadias Questionnaire). General demographic data, number of cases operated per year, preferred technique in the correction of hypospadias, outcomes and complications were gathered. The data was analyzed and compared with international practices.
Results: 75 surgeons responded to the questionnaire. Only 34.7% do > 20 cases a year. 41.3% do < 20 cases. Most (82.7%) operate at ≤ 2-year age. Only 30% operated at District or Government Health Care facilities. Majority (70%) operated in private General hospitals and Nursing Homes. Tabularized incised plate (TIP) is the preferred technique in distal hypospadias. In proximal hypospadias, two stage-repair is preferred. All use indwelling stents.
Complications: Overall, 80% had ≤ 20% complication rates. Coronal urethra-cutaneous fistula was the most common complication.
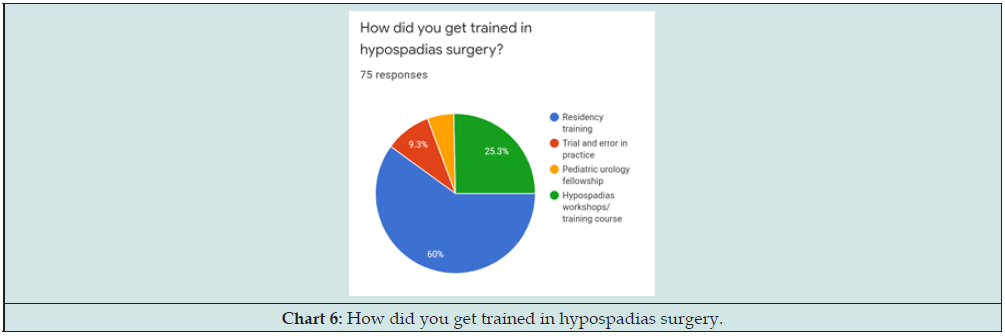
Training: 60% learnt hypospadias during residency; 35.6% learnt it through hypospadias workshops and training courses.
Conclusion: Hypospadias can be successfully managed in resource-limited settings; the single most limiting factor is the professional skill of the surgeon. There is an urgent need to extend pediatric surgical services to our rural government and district hospitals. COPS-IAPS is a step in this direction. This study contains data based on personal experience. Future research must focus on prospective controlled trials.
Keywords: Hypospadias; rural surgeon; district hospitals; survey
Introduction
Hypospadias is a common pediatric surgical problem with an incidence is about 1 in 250 male births [1] Factors that can influence choices in clinical practice include hypospadias severity, surgeon’s background, and preference [2,3]. Surgeons practicing in Rural and District Hospitals (First-Level Hospitals -Table 1) with limited-resources are faced with numerable challenges [4]. We try in our study to evaluate current practices regarding a variety of aspects of hypospadias surgery amongst pediatric surgeons at Rural Hospitals with emphasis on experience of surgeon, preferred technique & surgical training and to compare them with the international practices.
Materials and Methods
A multiple-choice online survey was distributed among a sample of 200 pediatric surgeons practicing at Rural and District Hospitals in Maharashtra State using Google Form application (HYPOSPADIAS QUESTIONNAIRE) between January and March 2019. It included questions about participants demographics, number of cases operated per year, surgical technique, intraoperative preferences, and complications. Data were analyzed and compared with international practices.
Results
A total of 75 Surgeons out of 200 responded to the online anonymous questionnaires.
Demographics
All 75 were Pediatric Surgeons practicing at Rural Hospitals - either District or Government hospitals / Private Hospitals or Nursing Homes.
Surgeons’ Experience
a) Practice experience (Chart 1): 60% are practicing pediatric surgery for more than 10 years. 20% are practicing for 5- 10 years and 20% for < 5 years.
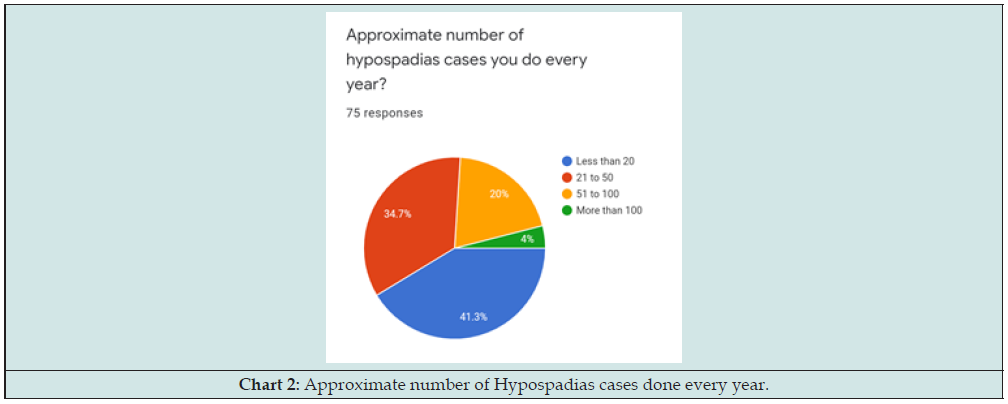
b) Workload (Chart 2): Large number (41.3%) do < 20 cases/ year. 34.7% are doing 21- 50 cases/ year. Only a Minority (20%) are doing 51-100 cases: only 3% respondents > 100 cases/year, qualifying the tag of hypospadiologist [5].
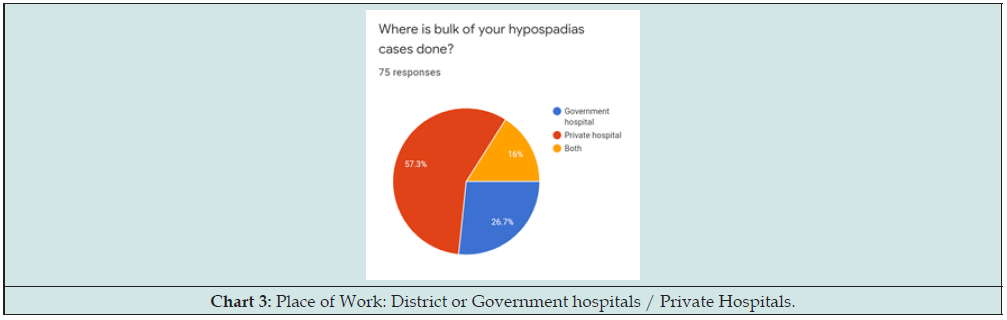
c) Place of Work (Chart 3): District or Government hospitals / Private Hospitals or Nursing Homes (First-Level Hospitals). The overwhelming majority (70%) operated in Private General hospitals and Nursing Homes; less than 30% operated at Government Health Care facilities.
d) Referral Pattern: 50% referred by pediatricians; 30% come directly.
Surgical Technique & Intra-operative Preference
Most (82.7%) operate at ≤ 2-year age; 17.3 % > 2 years. Important criteria for choice of operation (Chart 4) were Urethral Plate characteristics (70.7%), Chordee (57.3%), glans size (26%) and phallus size (29%).
Tabularized incised plate (TIP) is the preferred technique in distal hypospadias without chordee. In proximal hypospadias, two stage-repair is preferred. 76% try alternative methods of correcting the ventral penile curvature to preserve native urethral plate. The overwhelming majority (97.3 %) reported use of inner preputial skin as their choice for ventral graft during staged repair. Less than 3% use buccal mucosa, at least in primary cases. To prevent buccal mucosal graft contracture, 23% of respondents use topical steroids.
All 75 (100%) use indwelling catheters for draining the urinary bladder post operatively. 60.8% do single layer subcuticular urethroplasty; 30% do a 2-layer urethroplasty. Suture-Material: 65% prefer vicryl (polyglycolic-acid) for urethroplasty. Choice of dressing: 54.1%-*Compression Dynaplast (*Dr. S. Mane – Senior Pediatric Surgeon), 36.5%-simple gauze wrap, 9.5%-Tegaderm. Antibiotic choice: 50%-3rd generation cephalosporin, 29.7%-Augmentin/Amikacin, and 2%-No antibiotic.
Complications
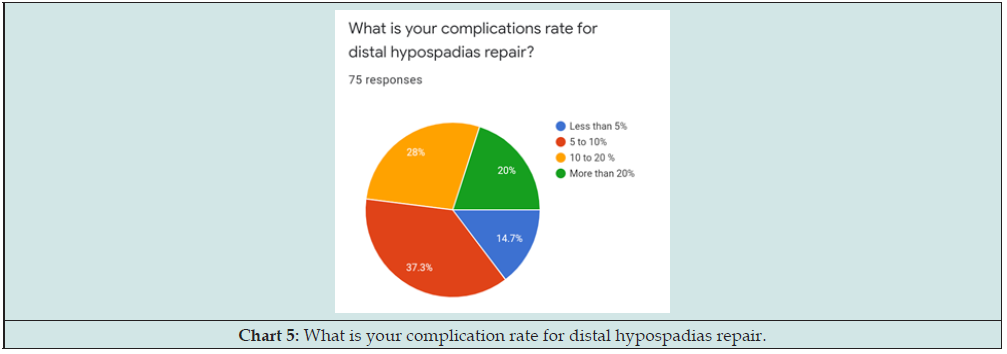
Overall, 80% respondents in our study had less than 20% complication rates; 37.3% reported 5-10% complications; 28% reported 10- 20% while 14.7% less than 5%. Urethro-cutaneous fistula was most common complication, 12.2%-meatal stenosis, and 9.5%-glans dehiscence (Chart 5).
Surgical Training & Operative Workshops
60% of surgeons learnt hypospadias surgery as part of residency training. 34.6% learnt through hypospadias workshops and training courses while less than 10% trained themselves during their practice by trial and error (Chart 6). Live Operative Workshops: 55% favored live operative workshop and 45% used edited video sessions as a tool for learning the nuances of hypospadias surgery.
Discussion
Hypospadias is a challenging field of urogenital reconstructive surgery, with different techniques currently being used. Prevalence varies across countries, races, and geographical locations with varying time periods. Pediatric Surgeons are better exposed to the principles of pediatric care during their residency training than any other surgical specialty. Also, nearly 30% of pediatric surgical training is already in pediatric urology [6,7]. Thus, Pediatric Surgeons unlike other surgical specialists (Adult Urology / Plastic Surgery) [8] are adequately equipped to handle these most common delicate genital anomalies where surgery is indicated early in life. What a Rural Surgeons can do in a resource-limited small place totally depends on his personal ability and facilities available to them. They face many limitations, which can be broadly divided into three, namely technical problems, professional skills, and legal problems. The single most limiting factor is the professional skill of the surgeon, which depends on the training he has received during his postgraduate studies and his desire and ability to implement them.
Technical problems can be due to non-availability of good and adequate equipment, facilities for investigations, non-availability of qualified paramedical personnel including qualified anesthetist and many others. But if one wishes, all these can be easily overcome. In our study we evaluated the current practices of hypospadias surgery amongst Pediatric Surgeons practicing in these resource-limited hospitals with emphasis on surgical training, preferred technique, experience of surgeon and outcomes compared to international practices. While there have been surveys in the literature evaluating surgeons’ practice in teaching institutions and urban areas, there are no publications to our knowledge evaluating current practices amongst surgeons practicing at Rural and District Hospitals. The questionnaire was sent to about 200 Pediatric Surgeons working at Rural Hospitals. 75 surgeons responded. Why so few people would respond to a simple questionnaire, where the identity of the respondent was not known, is difficult to understand. Medical community by default is an academic community, with never ending thirst for furthering the knowledge and continuous improvement of our treatment methods and techniques. We as a group need to inculcate this habit of participating in such surveys more often so we all benefit from the collective knowledge thus collected.
All the participants in our study were Pediatric Surgeons. This could be explained by a selection bias as the authors themselves are pediatric surgeons and could communicate effectively with peers. Rural vs Urban: 54.7% of our pediatric surgeons are practicing in Urban Metros and 41.3% in tier 2 and 3 cities [9,10]. Very few practices in rural hospitals. It is obvious that there is an urgent need to extend the pediatric surgical services to our rural areas where 50% of the population lives. Reaching out to Rural Areas: Community Oriented Pediatric Surgery Section (COPS) a subchapter of Indian Association of Pediatric Surgeons (IAPS) proposed an outreach program of pediatric surgery into health care policy, covering rural and tribal areas and collaboration with other specialists. With active participation of the IAPS executive council, Dr. Ravinder Vora, senior member from Sangli, Maharashtra, India, and Dr. Sudhakar Jadhav, past President, have taken steady steps toward this goal. A proposal has been submitted to the Rashtriya Bal Swasthya Karyakram in the Ministry of Health and Family Welfare (https://rbsk.gov.in/RBSKLive/), New Delhi, Delhi, India, wherein pediatric surgeons visit government hospitals in districts where pediatric surgical facilities are not available.
Government vs Private Hospitals: Surprisingly, about 70% respondents do majority of these cases in private hospitals and nursing homes. Government health care facilities, despite having a much bigger workload of patients, do not seem to be doing enough (30%). Outreach Surgical Services at District and Government Hospitals in Maharashtra: In Maharashtra, Dr. Ravindra Vora, senior pediatric surgeon & member IAPS has been successful in negotiation with government of Maharashtra to implement the pilot project. It is being implemented by *State Family Welfare Board, Pune. In the first phase 23 District Hospitals & 4 Government Hospitals have been included & there will be two regular visits to each hospital per month attending to outpatient clinics and operate planned cases.
Practice experience
One of the factors that are reported to be of paramount importance in the success of hypospadias surgery is the surgeons’ experience, and number of cases operated on per year [11]. Only one-third (34.7%) respondents are doing 21- 50 cases. It was noted that a large number (41.3%) of respondents do less than 20 cases a year. This is a woefully small number to achieve a significant expertise in this complex surgical procedure. In an international survey that included a cohort of 93 participants, 76% operated on ≥20 patients per year [12]. Many authors suggest that a minimum of 20 cases need to be operated on per year to be labeled as a highvolume hypospadias surgeon. Surgeons doing a very small number of cases (less than 10) per year should probably refer them to surgeons with a bigger case load and therefore more experience and expertise. Centralized practice of hypospadias surgery, especially severe defects and complex or re- do cases will improve the overall outcomes. Referral Pattern: 50% get references from general pediatricians and one third come directly to the pediatric surgeons for operation. This is an excellent sign of ideal practice making the population in general aware of the pediatric surgical problems. Surprisingly very few respondents get referrals from fellow pediatric surgeons or other surgeons. This needs to change. Surgeons doing < 20 cases/year having sub-optimal outcomes with significant percentage of complications should ideally refer to them to the hypospadiologist.
Surgical Technique & Intra-operative Preference were comparable with international practices
The most suitable age for operation of hypospadias is between 6 and 18 months. Another opportunity is at 3-4 years if the previous optimal age is missed [13]. Majority (82.7%) operate their cases before the age of 2 years. Only 17.2 % prefer to do it after 2 years, the reasons for which could be lack of expert anesthesia services and sophisticated instrumentation. Choice of Operation: John Duckett [14] had said “There are many successful methods, no single procedure works for all hypospadias cases, choose a suitable technique for individual case”. Factors that can influence choices in clinical practice include hypospadias severity, surgeon’s background, and preference. In distal hypospadias without significant chordee, Snodgrass [15] Tabularized Incised Plate Urethroplasty (TIP) is the preferred technique. In proximal hypospadias, the two-stage repair is most used which are standard international practices [16]. Intra-operative preferences such as technique of urethroplasty, use of stents, suture material, types of dressings and use of antibiotics also matched international practices.
Outcome and Complications were comparable with international practices
Overall, 80% respondents in our study had less than 20% complication rates; 37.3% respondents reported overall complication rate of 5-10% while it was 10- 20% for 28% respondents and 14.7% less than 5%. Coronal urethra-cutaneous fistula was the most common complication. The incidence of fistula that can be used to judge the success of hypospadias surgery ranging from 0% to over 35% which in our study is 20 % being comparable to other studies [17,18].
Training
60% learnt hypospadias as a part of their residency training. 34.6% learnt it through hypospadias workshops and training courses while less than 10% trained themselves during their practice by trial and error. If majority got trained during their residency, why the number of cases done in government hospitals is much less than private hospitals (as revealed by the respondents in another question) is difficult to explain (Image Letter).
Limitations and Final Remarks
Relatively small number of respondents from rural areas may have made this study less representative of overall pediatric surgical fraternity. A large number of more detailed questions could have been included in the study at the risk of making the questionnaire too long and respondent losing interest in completing and submitting. Why majority of hypospadias repairs are done in private hospitals when the general hospitals see many more patients is difficult to explain especially when majority of respondent reveal that they learnt their hypospadias surgery during residency training (which is done mainly in government hospitals and medical colleges). The surgeons with large patient load and experience in hypospadias surgery could formulate a standard operating procedure document on generally agreed upon parameters, which can serve as a ready reckoner for the younger, less experienced surgeons. Surgeons doing a very small number of cases (less than 10) per year should probably refer them to high volume centers for better outcome.
Conclusion
Proper and successful management of hypospadias can be enhanced by Pediatric Surgeons in resource-limited environment of Rural Hospitals overcoming most challenges. Surgeons in rural areas giving justice to needy and poor population should be appreciated and praised. There is an urgent need of extending the pediatric surgical services to our rural areas where 50% population lives. COPS-IAPS with cooperate is a step in this direction. Although data in this study come from reports of personal experience, it can serve as a guideline for future prospective studies on this topic.
References
- Bath AS, Bhandari PS, Mukerjee MK (2003) Repair of distal hypospadiasby tabularized incised plate urethroplasty: a simple versatile technique. Indian J Plast Surg 36(1): 23-25.
- Schröder A, Stein R, Melchior S, Fisch M, Riedmiller H, et al. (2006) Hypospadias. Urologe A 45: 204-208.
- Baskin L (2010) Editorial comment. J Urol 184(4): 1474-1475.
- Ajay D Subhedar, Shakuntala L Shelke, Sangita M Gavit (2016) Surgeries at rural hospital: From “Chekmate” to solutions. International Medical Journal 3(2): 117-122.
- Murphy JP (2010) Hypospadias. Ashcraft’s Pediatric Surgery. 5th ed. Philadelphia: Saunders Elsevier pp. 775-790.
- Gupta DK (1998) MCh Training program in pediatric surgery in India: Recommendations of the curriculum committee. Indian Association of Pediatric Surgeons.
- Hendren WH (1994) Pediatric surgery: Then and now. Arch Surg 129(4): 345-352.
- Raveenthiran V, Sarin Y, Bajpai M (2008) Pediatric Urology in India. Indian J Urol 24(3): 422-424.
- Rasik Shah (2015) The past, the present, and the future of pediatric surgery in India. J Indian Assoc Pediatr Surg 20(1): 2-7.
- Minu Bajpai (2016) Indian Association of Pediatric Surgeons Golden Jubilee: The milestone and the signposts ahead. J Indian Assoc Pediatr Surg 21(1): 1-5.
- Steven L, Cherian A, Yankovic F, Mathur A, Kulkarni M, et al. (2013) Current practice in pediatric hypospadias surgery; a specialist survey. J Pediatr Urol 9: 1126-1130.
- Timmons MJ (2010) The UK primary hypospadias surgery audit 2006-2007. J Plast Reconstr Aesthet Surg 63(8): 1349-1352.
- Manzoni G, Bracka A, Palminteri E, Marrocco G (2004) Hypospadias surgery when, what and by whom. Br J Urol 94(8): 1188-1194.
- Duckett JW (1995) The current hype in hypospadiology. Br J Urol 76: 1-7.
- Snodgrass W (1994) Tubularized, incised plate urethroplasty for distal hypospadias. J Urol 151(2): 464-465.
- Bhat A (2008) General considerations in hypospadias surgery. Indian J Urol 24(2): 188-194.
- Hardwicke J, Clarkson J, Park A (2007) Centralisation of a hypospadias repair service--the Warwickshire experience. J Plast Reconstr Aesthet Surg 60(1): 61-63.
- Snodgrass W, Villanueva C, Bush N (2014) Primary and Reoperative hypospadias repair in adults: are results different than in children? J Urol 192(6): 1730-1733.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...